Get full access with a free account
Benefits of the Coloplast® Professional Educational platform
![]() Full access to educational content, events and resources
Full access to educational content, events and resources
![]() Track your progress
Track your progress
![]() Share content with your colleagues
Share content with your colleagues
![]() Share supporting material with your patient
Share supporting material with your patient
The two conditions that lead to diabetic foot disease
Let’s take a look at how these two disorders lead to the formation of a diabetic foot ulcer.
Peripheral diabetic neuropathy – losing protective sensation
Peripheral diabetic neuropathy occurs when the sensory, motor and autonomic nerves of the peripheral nervous system don’t function properly in people with diabetes. Peripheral diabetic neuropathy is normally diagnosed when other causes have been excluded. Some patients experience painful sensory neuropathy, which includes a burning or tingling sensation known as paraesthesia.5
Peripheral diabetic neuropathy explained:
- is a result of poor glucose control
- is a common long-term complication in people with diabetes
- increases the risk of ulceration sevenfold
People with Peripheral diabetic neuropathy can’t feel:5
- temperature changes
- vibrations
- proprioception (i.e. the body’s movement or position)
- pressure
- pain
Peripheral arterial disease - injuries are slow to heal
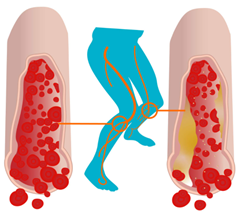
Peripheral arterial disease is another complication of diabetes. In Peripheral arterial disease, fatty deposits build up in the arteries. These deposits keep blood from flowing to the leg muscles.8 This lack of adequate blood flow prevents leg ulcers from healing.5 So when a chronic leg ulcer develops, this can lead to infection and amputation.
How do I know my patient has Peripheral arterial disease?
If your patient has diabetes, consider the following:
- Do they complain of weakness in the legs?
- Do they experience thigh or muscle pain or cramps (i.e. intermittent claudication) when walking?
If your patient answers ‘yes’ to these questions, he or she might have Peripheral arterial disease. The symptoms can range from asymptomatic to gangrene in the legs. However, most patients that have Peripheral arterial disease are not aware of it, so they don’t seek treatment.5
How Peripheral diabetic neuropathy affects blood flow
This picture illustrates how fatty deposits build up in the arteries. These deposits restrict the blood flow in the legs.
Did you know?
PAD is present in up to 50% of patients with a diabetic foot ulcer.
