Get full access with a free account
Benefits of the Coloplast® Professional Educational platform
- Full access to educational content, events and resources
- Track your progress
- Share content with your colleagues
- Share supporting material with your patient
Understanding pressure ulcers
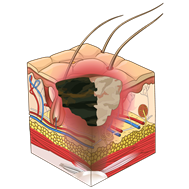
What is a pressure ulcer?
A pressure ulcer is localised damage to the skin and the underlying soft tissue. The injury is usually over a bony prominence or related to a medical or other device due to unrelieved pressure.
The pressure ulcer can:
- Present as intact skin or as an open wound
- Be painful
- Occur as a result of intense and/or prolonged pressure
- Occur as a result of pressure in combination with shear
A number of contributing or confounding factors are also associated with pressure ulcers: The primary of which are impaired mobility and impaired sensation
Who is at risk of developing pressure ulcers?
A number of risk factors can lead to the development of pressure ulcers.
Intrinsic factors
- Malnutrition or dehydration
- Vascular disease
- Circulatory abnormalities
- Multiple co-morbidities
- Previous history of pressure ulcer
- Neurological conditions
- Sensory impairment
- Acute illness
- Level of consciousness
- Extremes of age
Extrinsic factors
- Surface the patient is nursed on
- Reduced mobility or immobility
- Moving and handling aids/ techniques
- Medication – sedation
- Length of surgical procedures
- Devices used i.e oxygen , plaster of Paris, intubation
- External influences on the skin such as Urine, Faeces, Excess talcum powder, perfume, starch or over use of soap and massage or rubbing
How are pressure ulcers classified?
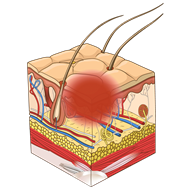
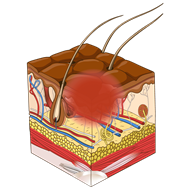
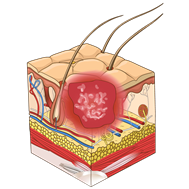
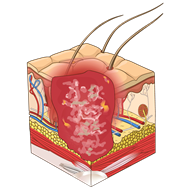
This illustrations below show the total of 6 descriptors that describe the depth of a pressure injury. The first four are described as “stages” or categories ranging from one to four. The last two additional stages are called “unstageable” and “Deep tissue injury.”
| Category 1 pressure ulcer: Non-blanchable erythema in fair skin | Category 2 pressure ulcer: Partial thickness skin loss |
|---|---|
|
|
|
| Category 3 pressure ulcer: Full thickness skin loss |
Category 4 pressure ulcer: Full thickness skin and tissue loss |
|---|---|
|
|
|
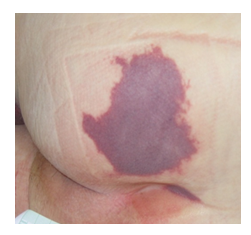
| Unstageable pressure ulcer: Depth unknown |
Deep tissue injury: Depth unknown |
|---|---|
|
|
|
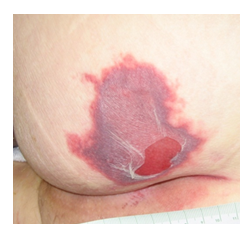
What is Moisture Associated Skin Damage (MASD)?
One of the commonest reporting errors is around moisture lesion. Clinicians can associate this damage with pressure and grade these lesions Category II to IV
- Often caused by incontinence associated dermatitis (IAD) due to exposure to urine of faecal matter, but can be caused if excess exudate or perspiration present
- Most commonly present in natal cleft
- Loss of epidermis and skin appears macerated, red, broken and painful
- Presents as a ‘kissing’ ulcer or a superficial red diffuse skin break
- Irregular shape
- Without necrosis
- Not directly over a bony prominence

What are the key risk factors for Incontinence Associated Dermatitis (IAD)?
The increase in moisture resulting from episodes of incontinence, combined with bacterial and enzymatic activity, leads to the breakdown of vulnerable skin, particularly in those who are very young or elderly.
Intrinsic factors
- Faecal incontinence (diarrhoea/formed stool)
- Double incontinence (faecal and urinary)
- Urinary incontinence
- Frequent episodes of incontinence (especially faecal)
- Poor skin condition (e.g. due to aging/steroid use/diabetes)
- Diminished cognitive awareness
- Pain
- Raised body temperature (pyrexia)
- Medications (antibiotics, immunosuppressants)
- Poor nutritional status
- Critical illness
Extrinsic factors
- Use of occlusive containment products
- Poor manual handling resulting in increased friction
- Inability to perform personal hygiene
- HCP and social care involvement
- Concordance
- Type of cleansing products used and method adopted
What's the difference between pressure ulcers and MASD
| Pressure Ulcer | MASD (incl moisture lesions) | |
|---|---|---|
|
Cause |
Pressure and/or shear forces internal or external |
Moisture( MASD): incontinence (incontinence associated dermatitis), sweat( intertrigininous dermatitis/Intertrigo, peristomal(stoma), periwound(wound exudate and friction |
|
Location |
Usually bony prominence, occuring in a defined area |
Sacrum, perineum, stoma, wound edges, skin folds, any part of the body exposed to moisture |
|
Depth |
Superficial to full thickness |
Superficial to partial thickness |
|
Shape |
Defines edges, often circular or irregular shape |
Diffuse area (moisture uncontained). ‘Kissing’ ulcers may be present |
|
Necrosis |
Possible necrosis |
No necrosis |
|
Colour of wound bed |
Non blanching erythema, Slough, Necrosis |
Red, pink or white. Not equal |
Did you know?
200,000 people have chronic wounds in the UK of which pressure ulcers are the single most costly chronic wound to the NHS1
Pressure Ulcers account for up to 4% of the UK healthcare budget, or £2,1 billion/year2
Pressure ulcers in older patients are associated with a fivefold increase in mortality, and in-hospital mortality in this group is 25% to 33%3
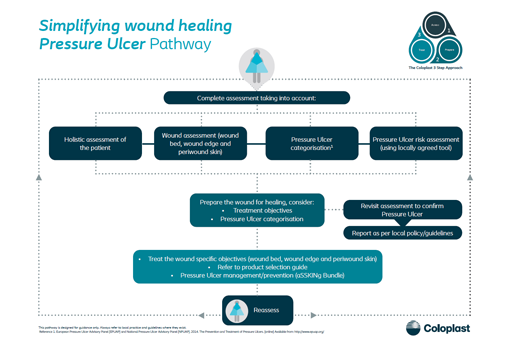
Pressure Ulcer Pathway
Using the Coloplast 3 Step Approach, we've broken down the process for Assessing, Preparing and then treating pressure ulcers into a simplified pathway.
Stop Pressure Injury Day
At Coloplast we are supporting the worldwide goal to Stop Pressure Injuries.
In this video we explore some of the key challenges and what we should do to stop pressure injuries.
Skin care: Incontinence interventions
Skin exposed to urine and stool increases the risk for incontinence associated dermatitis (IAD) and pressure ulcer development.14
Cleanse the skin promptly following episodes of incontinence.14,15
Cleanse, moisturise and protect:
- Skin should be cleansed with a pH-balanced cleanser to maintain the acid mantle
- Consider using a skin moisturiser to hydrate dry skin
- Protect the skin from exposure to urine, stool and excessive moisture with a moisture barrier
Consider the use of urinary catheters or faecal containment devices for high risk individuals.
Evolution of deep tissue injury examples
In these 3 clinical pictures you see how a sacral pressure injury fairly rapidly can progress.
Day 1 – The skin is intact but discolored, this stage is to be classifies as a Deep Tissue Pressure Injury
Day 3 – The skin is still discolored with epidermal blistering. The stage is still a Deep Tissue Pressure Injury
Day 10 – The Deep Tissue Injury (DTI) has become necrotic and covers the pressure injury, therefore it is now classified as an Unstageable Pressure Injury
Deep Tissue Injury - Day 1
Deep Tissue Injury - Day 3
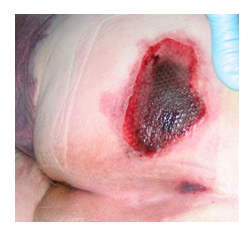
Deep Tissue Injury - Day 10
Browse our educational E-learning courses

Pressure Injury Management
In this course you will learn about how to assess and manage pressure injuries.

Pressure Injury Prevention
In this course you will learn how to classify pressure injuries, how to examine and assess the patient's skin as well as get techniques for preventing pressure injuries.
Bite sized education
Educational module on pressure ulcers, their impact and implications. What causes them and some of the most common locations.
Patient cases

Pressure Ulcer on the right lower limb
Read how the pressure ulcer was treated, leading to granulation tissue in 56 days.

Treatment of recurring pressure ulcer over the left ischium with a silicone foam dressing
Read how the pressure ulcer was treated, leading to reduced wound size by almost 50% within 29 days.
Clinical videos
Assessment & management of a Pressure ulcer on the right heel
See how the Triangle of Wound Assessment is used as a tool to assess a Pressure ulcer
Treatment of a Pressure Ulcer with a silicone foam dressing
See how a pressure ulcer on the right lower leg progresses toward wound healing in 56 days.