Get full access with a free account
Benefits of the Coloplast® Professional Educational platform
- Full access to educational content, events and resources
- Track your progress
- Share content with your colleagues
- Share supporting material with your patient
Did you know?
A study in 2015 found that there were at least 730,000 patients with leg ulcers in the UK, which equates to 1.5% of the adult population having a leg ulcer.
It is well recognised the ulcers as a result of underlying venous disease are the most common aetiology of leg ulceration.
The number of diagnosed venous leg ulcers (VLU) indicates that 1 in 170 adults have a VLU.
Understanding Venous Leg Ulcers
What is a venous leg ulcer and why does it occur?
A venous leg ulcer (VLU) is an open skin wound, or lesion, and that shows little progress towards healing within 4-6 weeks of when it initially occurred. Venous leg ulcers usually occur between the ankle and the knee (medial side of the lower leg) and are the most common type of chronic lower limb wound.1
Venous leg ulcers are caused by disease or disrupted vein function, also known as chronic venous insufficiency (CVI) and ambulatory venous hypertension. chronic venous insufficiency usually results from damage to the valves in the leg veins (for example, varicose veins) or as a result of venous thrombosis.1
Ambulatory venous hypertension occurs in patients with varicose veins, when there is an inadequate decrease in venous pressure while walking and exercising.
What causes leg ulcers?
Most leg ulcers are associated with a circulatory disorder. Venous, arterial and mixed aetiology will account for 90-95% of all leg ulcers1.
Common causes of leg ulcers
- Venous
- Arterial
- Mixed venous and arterial
- Traumatic
Less common causes of leg ulcers
- Vascultis causes
- Malignancy
- Necrobiosis lipoidica diabeticorum
- Pyoderma gangrenosum
- Infection including tropical ulcers
- Psychosocial
- Self-induced injury
How do I manage venous leg ulcers?
Research shows that compression therapy is the key to managing venous leg ulcers. Compression therapy increases healing rates when compared to non-compression therapy. And after healing, it reduces the rate of recurrence.
You can consider all lower limb wounds that are either caused by venous disease or have venous disease as a part of a mixed aetiology, as potential candidates for compression therapy.1
What are the recurrence rates for venous leg ulcers?
Recurrence rates of leg ulcers are high and once healed there is a great risk of recurrence.
12 months recurrence between 26% and 69%1
70% recurrence in patients not fitted with compression hosiery2
How are patients impacted?
VLUs have been found to have a significant impact on patients’ quality of life, with associated personal, social and psychological effects.
Potential for significant financial burden on the patient.1
Pain is a significant factor and is often underestimated leading to poor management.2
Accurate assessment is crucial in ensuring correct treatment.
Definition of a leg ulcer
Wound to the lower leg that remains unhealed after 4-6 weeks (1,2) as a result of underlying aetiology.
A leg ulcer is not a disease, but a symptom of a disorder.3
Sound knowledge of the skin, lymphatics and vascular systems is essential to understand the aetiologies, prevalence and management of leg ulceration.4
“An open lesion between the knee and the ankle joint that occurs in the presence of venous disease and takes more than two weeks to heal”
If present for 2 weeks, assess for suitability for compression.
Immediate treatment with compression if indicated.
How to treat a leg ulcer
Treatment of a leg ulcer should be directed at the underlying cause.
- Venous insufficiency: increasing venous blood flow back to the heart
- Arterial disease: improving arterial blood flow to the leg
- Management of other co morbidities including glycaemic control
Appropriate referral to specialists:
- Vascular surgeon
- Diabetologist
- Medical specialty
- Dermatologist
Treatment of venous disorders with compression therapy
The key to healing a venous leg ulcer and preventing recurrence is the use of graduated compression therapy.
| Reduce pressure difference → | Force the fluid back → |
Increase velocity and flow → |
Valves close and functions |
|---|
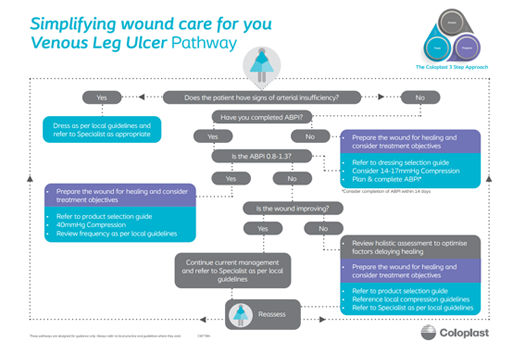
Venous Leg Ulcer Pathway
Using the Coloplast 3 Step Approach, we've broken down the treatment process for Assessing, Preparing and then treating a venous leg ulcer into a simplified pathway.
References
- Harding K, et al. Simplifying venous leg ulcer management. Consensus recommendations. Wounds International 2015
- Wounds UK (2019) Best Practice Statement: Addressing Complexities in the Management of Venous Leg Ulcers. London: Wounds UK. Available to download from: www.wounds-uk.com
- Diehm, C., Schuster, A., Allenberg, J.R. (2004). High Prevalence of Peripheral Arterial Disease and Co-Morbidity In 6880 Primary Care Patients: Cross-Sectional Study. Artheroclerosis; 172: 95-105
- Nelson, A. and Adderley, U. (2016). Venous Leg Ulcers. Clinical Evidence 01, 1902
Webinars & E-learning

Facebook Live, 17th Dec 2020
Transforming Wound Care. Simplifying venous Leg Ulcer management

Leg Ulcers
In this E-learning course you will learn how to identify, assess, and manage leg ulcers.
Patient Cases
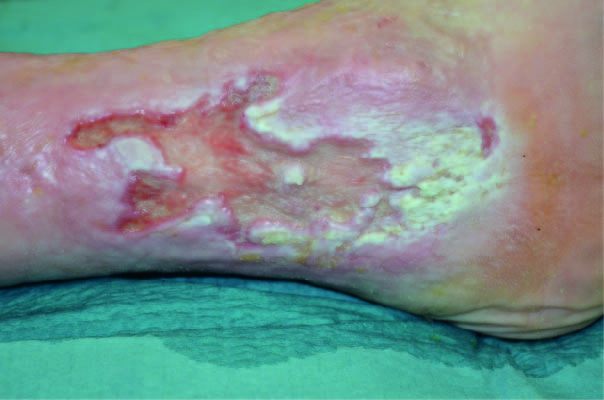
Treatment of a macerated Venous Leg Ulcer
See how a macerated venous leg ulcer was treated with a silicone foam dressing.

Treatment of an Arterial Leg Ulcer on lower leg
Read how a colonized arterial wound was treated in a wound clinic.
